Especially now, as we come out of a very difficult past 12 months, occupational health practitioners are not immune to the impact of their work, with some experiencing high levels of clinical symptoms, including anxiety, depression, traumatic stress and burnout. Online psychological screening and surveillance can help, as Noreen Tehrani and Lorraine Anderson-Cole explain.
Back in 2014 I wrote an article on psychological screening and surveillance in the workplace that was published in Occupational Health & Wellbeing. Much has been learnt during the past six years, so it seemed appropriate to revisit the topic and bring the knowledge of occupational health professionals up to date.
Health screening and surveillance
The role of occupational health (OH) is to protect and promote the health of workers by preventing and controlling occupational disease (WHO, 1994).
Occupational health professionals employ a health surveillance approach to the collection, analysis, recording and interpretation of health-related data in the screening employees for hearing, sight, and physical fitness (Freeman, Colpe et al, 2010).
Organisations have a legal requirement to undertake health surveillance (HSE, 2009) which involves the detection of ill-health effects; the introduction of controls to prevent harm; the provision of data to evaluate health risks and raise concerns; the highlighting of failures of control measures; and the provision of feedback and opportunities to reinforce health and wellbeing through training and education.
Until recently, most health surveillance has focused on physical health. However, since 1996 it was legally established (Page v Smith 1996) that physical and psychological health should be treated equally.
For more than 20 years it has been necessary for organisations to undertake both physical and psychological surveillance of employees. The World Health Organization (WHO 1994) has described the aim of health surveillance to be the elimination of occupational factors and conditions hazardous to health and safety at work. It has placed a focus on creating healthy and safe work, working environments and organisations to support workers to live socially and economically productive lives.
There are two separate but complementary health surveillance processes. The first is psychological hazard surveillance involving the identification, elimination, reduction and management of hazards. The second is psychological health surveillance, or the assessment of clinical symptoms in individual and groups of workers.
The identification of psychological hazards and the assessment of clinical symptoms employ similar types of questionnaires and assessments. However, it is important that OH professionals do not confuse these two processes and are able to differentiate the tools and processes used for assessing workplace hazards from those used for clinical assessment and diagnosis. We’ll now look at health surveillance process in turn.
Psychological hazard assessment
Psychological hazard surveillance uses a range of tools and approaches to identify hazards. This can include individual and group discussions, wellbeing checklists and questionnaires. However, there is an increasing adoption of regular online questionnaires and surveys.
The World Health Organization (WHO, 2008) and the Health and Safety Executive (HSE, 2014) have identified a range of psychosocial hazards in organisations. These include damaging organisational policies, culture and industrial relations and employee conditions, job design, work demands, control and relationships. There are many questionnaires designed to measure organisational and individual factors shown to impact individual psychological wellbeing.
One group of questionnaires focuses on hazards that increase the risk of psychological ill health (Tehrani & Hesketh, 2019) and include measures for traumatic exposure, neuroticism, bullying, adverse childhood experiences, external locus of control and substance abuse.
A second group has been are more concerned with resilience or coping factors. These include the “COPE” inventory (Carver et al, 1989), “Workability” (Ilmarinen, 1991), “Resilience Scale” (Connor & Davidson, 2003), Sense of Coherence (Antonovsky, 1979) and Psychological Wellbeing (Joseph et al, 2012).
Occupational health professionals should be aware of the risk of over-interpreting results when measuring hazards in individuals. Nevertheless, there is strong evidence that these factors are strong indicators of future wellbeing, with the ability to predict the negative outcomes. Uncontrolled psychological hazards can increase accidents, absence, turnover and presenteeism in groups and organisation. However, the presence of a hazard should not in itself be used to predict the development of disease in an individual.
For example, just as not everyone who smokes will develop lung cancer, not everyone exposed to a traumatic event will develop post-traumatic stress. Equally, it would be discriminating to use an individual’s gender, personality, childhood experiences or limited coping skills in recruitment and selection, as the data is an unreliable predictor for individuals (Equalities Act, 2010).
The benefit of undertaking hazard surveillance is to work to reduce or eliminate the impact of the hazard on workers with health promotion, education and training programmes.
Clinical psychological health assessments
Psychological health surveillance involves a periodic assessment of clinical symptoms in high risk groups. The surveillance process provides opportunities for the early detection of mental health problems and enables proactive preventative measures or treatments to be provided.
Clinical surveillance can involve use of self-report clinically validated questionnaires and clinician administered assessments. When selecting a clinical measure, it is important to ensure the questionnaires are reliable, valid, accurate and with clear cut-off levels and the clinician undertaking the assessment has the required level of qualification and experience, (BPS, 2020).
A difficulty in undertaking psychological surveillance is created in organisations where there are high levels of mental health stigma. Where employees fear giving honest responses as this may affect their job or opportunities at work, this can result in some providing overly positive and inaccurate results.
To some extent, this can be identified by including a social desirability questions identifying people scoring this way. Alternatively, it is also possible to include questions on stigma. A number of studies in the military (Acosta et al, 2014) and with first responders (Haugen et al, 2017) have shown up to 30% of responders believe there is a mental health stigma in their organisation.
In UK policing, only 3% of officers and staff reported significant stigma in their teams, with 14% reported a little stigma. This evidence suggests that, although stigma may be an issue, it may be less frequent in those taking part in surveillance programmes.
The benefits of psychological surveillance
| Measure the prevalence of occupational disease
Indicate the presence and absence of a hazard Assess the adequacy of control measures Identify workers at increased risk |
Establish baseline symptom levels
Provide benchmarks for preventative action Identify opportunities for health education Evaluate the benefit of wellbeing interventions |
In the past five years, over 20,000 UK police officers and staff have taken part in psychological surveillance programmes. Over the past two years, the College of Policing has funded psychological surveillance for some policing roles. These include firearms’ officers, negotiators, family liaison officers and those dealing with online child abuse (and see oscarkilo.org.uk for more on this).
This programme is offered through occupational health departments and supported by occupational health advisors (OHA) and counsellors (OHC) trained in undertaking structured psychological interviews.
The screening is of two types, surveillance which is typically involves the completion of an annual online screening, and referral screening, which is used to assess the psychological symptoms and wellbeing hazards for people identified as experiencing difficulties.
In line with HSE guidance, surveillance is only carried out with employees in roles assessed as being at risk of mental health problems, including anxiety, depression, primary and secondary trauma (Tehrani and Hesketh, 2019).
The results from the surveillance of the 20,000 police showed 80% to be fit, 15% to be requiring advice or support and 5% with significant clinical symptoms.
The officers requiring support are taken through a structured interview by OH professionals and, using the results of the screening, are able to provide targeted guidance on ways to address problems with lifestyle, coping skills, relationships, or other work-related issues.
The officers with the highest levels of clinical scores are seen by psychologists, who undertake a full psychological assessment and then provide a written report, opinions, and management advice.
Surveillance in the international military
Although there are significant differences between the experiences of police and military personnel, when involved in armed combat soldiers are exposed to high levels of stress and trauma.
It is therefore not surprising that most countries have adopted psychological surveillance for military personnel at three points in time: pre deployment, during deployment and post deployment.
Warner et al (2011) undertook an evaluation of the effectiveness of psychological screening involving over 21,000 soldiers, with approximately half being screened and the others unscreened, as shown in figure 1. The results showed significant reduction in mental health problems, in medical evacuations from Iraq for mental health problems and in suicidal ideation in the screened groups.
Figure 1. Pre-deployment screening in the US military
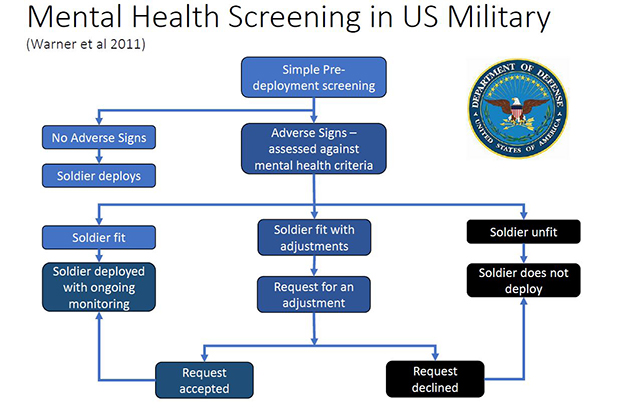
The US military model is similar to that adopted in UK policing. However, where UK police officers and staff are identified as having clinically significant symptoms, every effort would be made to help them remain in policing employment and offered trauma therapy, rehabilitation plans, and temporary or permanent adjustments to their roles.
In the military, personnel were more likely to be medically discharged rather than offered adjusted duties and psychological rehabilitation.
Surveillance and management information
Although the information gathered from psychological screening and surveillance is useful in assessing and treating individuals it also lends itself to the creation of management information.
The surveillance data can be used to benchmark groups and teams and provide longitudinal trends. The data can also be used to show the influence of changes in management, benefits of training or system updates.
The management data can identify the influences of psychological hazards and resilience on clinical scores. The anonymised dashboard (figure 2) provides an illustration of some of the management information generated from the police surveillance programmes.
The red bar shows the benchmark which is the average results for over 20,000 assessed roles. In this example, the completion rate is around average and the fitness rate has improved year on year as can also be seen in all the major clinical symptoms. However, the levels of secondary trauma, anxiety and depression are higher than benchmark.
Figure 2. Anonymised illustration of management information over three years
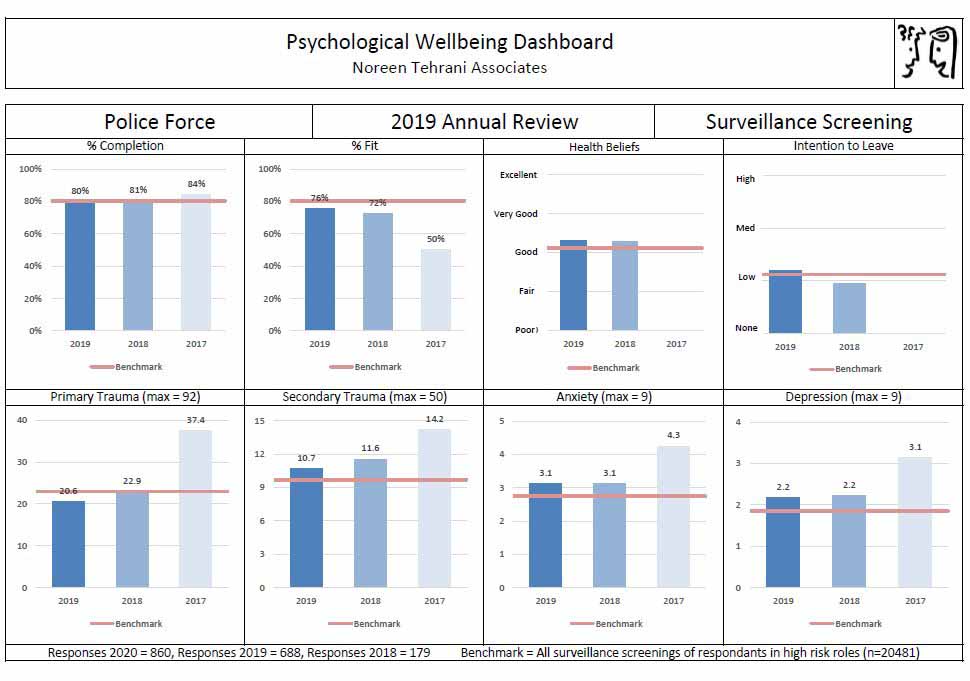
The second set of results shows this group is on benchmark with regards the “Sense of Coherence” (Antonovsky, 1979), in which meaningfulness, managability and comprehensibility are strong resilience factors.
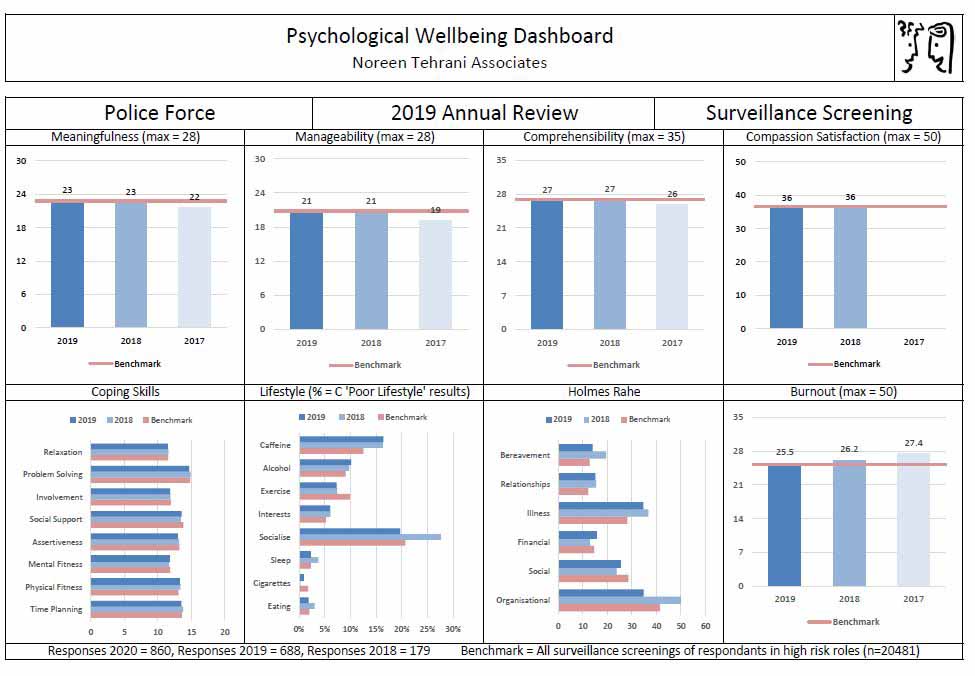
The results show a high level of compassion satisfaction. The lifestyle results (figure 3) show a need for more socialisation and a reduction in caffeine containing drinks, and Holmes Rahe shows that organisational issues are the main sourse of stress.
Figure 3. Additional anonymised management information from screening
Psychological surveillance in the NHS, social care and policing
The Covid-19 virus, as we all know, recognises no boundaries or borders and by the beginning of 2021 had killed well over two million people.
People are being asked to be physically screened for the virus and virus antibodies. At the same time, there is a growing recognition of the impact the pandemic is having on mental health.
In the UK there are approximately 1.2 million NHS and 1.6 million social care workers. It has been suggested (BMA, 2020) that as many as 20% of NHS workers are experiencing psychological difficulties due to their work; it is possible over half a million people may need support with over 100,000 requiring treatment for anxiety, depression or traumatic stress.
Without comprehensive psychological screening, it is difficult to see how this group of people can be identified and provided with the treatment they need. The University College London Covid Trauma Response Group (UCL Covid Trauma Response Group, 2020) has called for a national “screen and treat” service managed through regional mental health screening programmes for members of the public. It seems logical that OH services should be seeking similar facilities for NHS and social care workers.
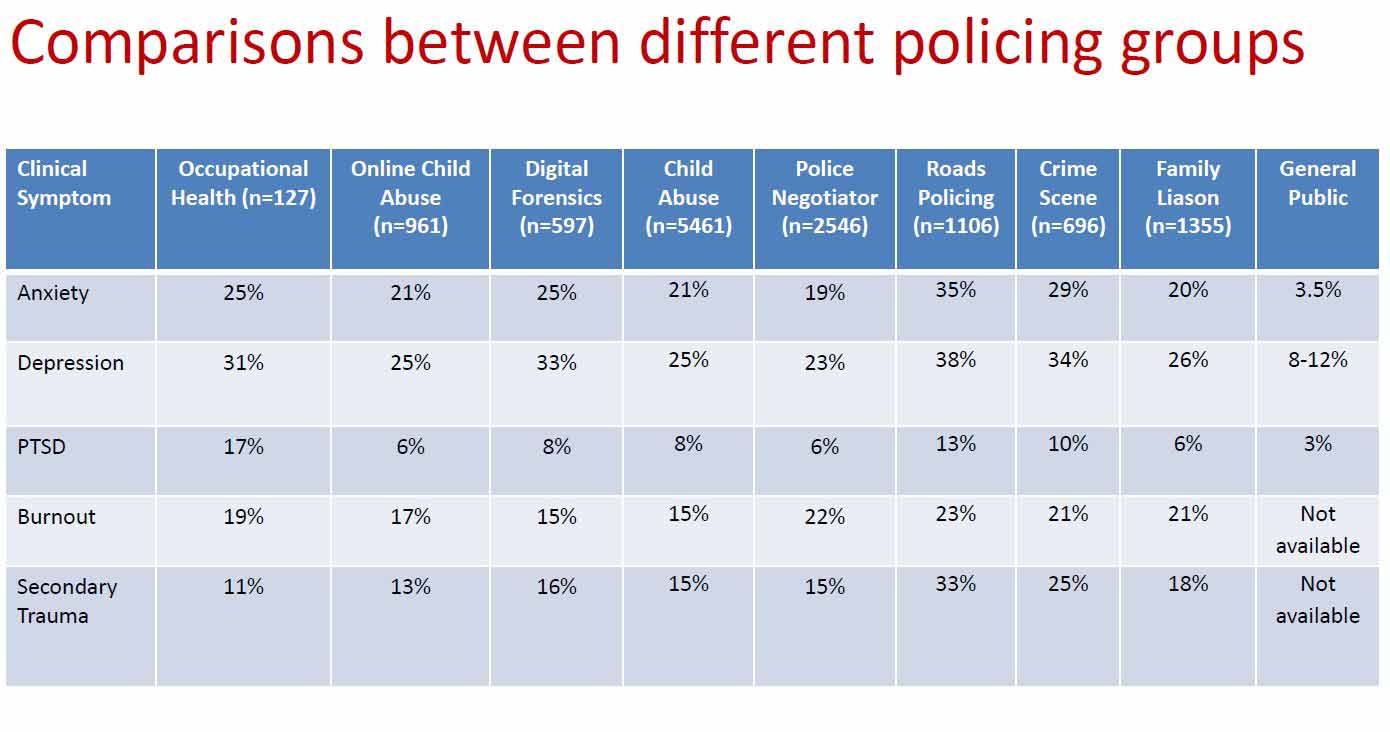
A psychological surveillance survey of occupational health practitioners (OHPs), undertaken as part of a training programme (Oscar Kilo, 2020), found that, in a group of 127 OHPs, a quarter had clinically significant symptoms of anxiety. Almost a third had significant levels of depression, 17% had PTSD, 19% burnout and 11% secondary trauma.
These results indicate OH practitioners working in policing are at a higher risk of developing PTSD than their policing colleagues and also experience high levels of anxiety and depression.
The following table (figure 4) compares the psychological screening results of the OHPs with a number of policing roles, including officers dealing with online child abuse, crime scene investigations, family liaison and child abuse. A comparison is made with the levels found in the general public.
Figure 4. Comparison between occupational health practitioners, other workers and the general public
Occupational health practitioners engage directly with workers experiencing physical and psychological difficulties. However, it appears that few are supported in taking care of their psychological wellbeing (Dovey, Smith & Anthony, 2020).
Need for clinical supervision for occupational health practitioners
Clinical supervision for occupational health nurses was identified as important by the Royal College of Nursing Occupational Health Managers’ Forum (RCN, 2002) within the Normative, Formative and Restorative Framework developed by Proctor (1986).
Proctor’s framework involves the development of skills and knowledge (formative) exploration of emotional reactions and responses (restorative) and maintenance of standards (normative).
However, unlike other professional groups where clinical supervision is mandatory, occupational health practitioners and OH services are not required to provide clinical supervision.
Despite the lack of formal clinical support offered by OH services, many OHAs create informal “peer supervision”; however, this is often unsupported by the allocation of protected supervision time or clinical supervision training.
In the past, the focus of clinical supervision in nursing has been the normative monitoring; the practice and delivery of improvements in patient care. There has been little emphasis on the practitioner restoration, which is important in assuring the psychological health safety and wellbeing.
In policing, clinical supervision programmes have adopted by some police forces, including Cumbria Constabulary where the occupational health advisors and manager have regular supervision from an occupational health psychologist.
The supervision sessions are designed to meet the normative, formative and restorative needs of the OH team. The Cumbria approach is supported by the College of Policing Foundation Standards in Occupational Health (College of Policing, 2019 p11). This recommends there should be systems in place “to provide regular support and clinical supervision for OH teams with access to internal trauma support”.
Models of restorative supervision have also been developed by the College of Occupational Therapists (2015) and Health Visitors (Wallbank, 2012). These programmes have recognised the need to address the emotional demands of staff working in these environments and to provide ways to reduce stress and increase job satisfaction.
A number of NHS trusts have introduced Schwartz rounds (Cullen, 2016), which provide a platform for clinicians and staff to share the emotional impact of working in demanding and emotionally draining environments.
Whilst some attendees report a benefit from these sessions, Schwartz Rounds should not be regarded as a substitute for clinical supervision and may be harmful if not delivered by trained and experienced facilitator.
A study looking at beliefs and attitudes of occupational health advisors to their work established that formal clinical or peer supervision can transform negative experiences and stressors (Tehrani, 2010).
Supporting the psychological health and wellbeing of occupational health practitioners in a way that provides an opportunity for reflective practice and can increase learning, development and psychological wellbeing.
Conclusions
There is a legal requirement to undertake psychological surveillance of employees working in roles which pose a significant recognised risk to mental health.
Occupational health practitioners are not immune to the impact of their work, with some experiencing high levels of clinical symptoms including anxiety, depression, traumatic stress and burnout.
Online psychological screening and surveillance is an effective way to identify workers in need of support. But it is also important to differentiate between psychological health surveillance, which measures clinical symptoms that may require treatment, and hazard surveillance, which identifies factors that indicate an increased vulnerability to developing psychological ill health where there is a need to address the impact of the hazard.
We believe there is an important role for psychological surveillance in organisations, and that some OHAs should also be in regular surveillance programmes and have access to restorative clinical supervision to mitigate the impact of working with troubled employee and organisations.
- With thanks to Caroline Russell, occupational health, safety and mellbeing manager at Cumbria Police, for her support and encouragement in developing psychological surveillance in policing.
References
Acosta, J D et al (2014). “Prevalence of Mental Health Stigma in the Military”, in Mental health stigma in the military, Santa Monica, Calif. Rand Corporation. Available online at: https://www.rand.org/pubs/research_reports/RR426.html
Antonovsky A (1979). “Health, stress and coping”. San Francisco: Jossey-Bass.
“Long-term impact of COVID on NHS must not be underestimated”, BMA May 2020. Available online at: https://www.bma.org.uk/bma-media-centre/long-term-impact-of-covid-on-nhs-must-not-be-underestimated
“The BPS qualifications in test use”, The British Psychological Society (2020). Available online at: https://ptc.bps.org.uk/sites/ptc.bps.org.uk/files/forms/2020_quals_in_test_use_flyer_general.pdf
Carver C S, Scheier M F, and Weintraub J K (1989). “Assessing coping strategies: A theoretically based approach”. Journal of Personality and Social Psychology, 56, pp.267-283. Available online at: https://pubmed.ncbi.nlm.nih.gov/2926629/
“Supervision: guidance for occupational therapists and their managers”, College of Occupational Therapists (2015). Available online at: https://www.rcot.co.uk/sites/default/files/Supervision.pdf
College of Policing (2019). National Police Wellbeing Service, Foundation Occupational Health Standards for Police Forces. Available online at: www.oscarkilo.org.uk/app/uploads/2020/02/Foundation-OH-Standards-for-Police.pdf
Connor K M, and Davidson J RT (2003). “Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC)”. Depression and Anxiety, 18(2), pp.76-82. Available online at: https://onlinelibrary.wiley.com/doi/pdf/10.1002/da.10113
Cullen A (2016). “Schwartz rounds: promoting compassionate care and healthy organisations”, Journal of Social Work Practice 30, 2, pp.219-228. Available online at: https://www.tandfonline.com/doi/abs/10.1080/02650533.2016.1168386
Dovey A, Swift M, Anthony P (2020). “Protecting occupational health practitioners from burnout,” Occupational Health and Wellbeing, March 2020. Available online at: https://www.personneltoday.com/hr/protecting-occupational-health-practitioners-from-burnout/
Equalities Act (2010), Gov.uk, https://www.gov.uk/guidance/equality-act-2010-guidance
Freeman E J, Colpe L J, Strine T W, Dhingra S, McGuire L C, Elam-Evans L D et al. “Public health surveillance for mental health” (2020). Prevention of Chronic Disease, 7 (1), pp.1-7. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2811512/
Haugan P T et al (2017). “Mental health stigma and barriers to mental health care for first responders: a systematic review and meta-analysis”, Journal of Psychiatric Research, 94, pp.218-229. Available online at: https://pubmed.ncbi.nlm.nih.gov/28800529/
HSE (2009). “Health Surveillance: a time for change”, Health and Safety Executive. Available online at: https://www.hse.gov.uk/research/rrhtm/rr810.htm
HSE (2014). “Risk assessment: A brief guide to controlling risks in the workplace”, Health and Safety Executive. Available online at: https://www.hse.gov.uk/pubns/indg163.htm
Ilmarinen, J (1991). “The aging worker”, Scandinavian Journal of Work, Environment & Health, 17 (sup. 1) pp.1-14. Available online via https://www.jstor.org/stable/i40043304
Joseph S, Maltby J, Wood A M et al (2012). “Psychological Well-Being – Post-Traumatic Changes Questionnaire (PWB–PTCQ): Reliability and validity”. Psychological Trauma: Theory, Research, Practice and Policy, 4(4), pp.420-428. Available online at: https://psycnet.apa.org/record/2011-17454-001
Oscar Kilo (2020). “Responding to trauma in policing: a practical guide”, www.oscarkilo.org.uk. Also available online at: https://www.college.police.uk/What-we-do/Support/Health-safety/Documents/Responding-to-trauma-in-policing.pdf
Page v Smith [1995]. House of Lords, UKHL 7.
Proctor, Brigid (1986). “Supervision: A co-operative exercise in accountability”, in Marken A and Payne M (eds), “Enabling and Ensuring: Supervision in Practice”, Leicester National Youth Bureau/Council for Education and Training in Youth and Community Work. Available online at: https://www.scirp.org/(S(i43dyn45teexjx455qlt3d2q))/reference/ReferencesPapers.aspx?ReferenceID=1547577
RCN (2002). “Clinical Supervision in the workplace: guidance for occupational health nurses”, Royal College of Nursing. Available online at: https://docplayer.net/3374564-Clinical-supervision-in-the-workplace.html
Tehrani N (2014). “CPD: A guide to psychological screening and surveillance in the workplace”, Occupational Health & Wellbeing, 2014, https://www.personneltoday.com/?p=126617
Tehrani N (2010). “Compassion fatigue: experiences in occupational health, human resources, counselling and police”, Occupational Medicine; 60, pp.133-138. Available online at: https://academic.oup.com/occmed/article/60/2/133/1423081
Tehrani N and Hesketh I (2019). “The role of psychological screening for emergency service responders”, International Journal of Emergency Services, vol. 8 no. 1, pp.4-19. Available online at: https://www.researchgate.net/publication/328206469_The_role_of_psychological_screening_for_emergency_service_responders
“COVID-19: National PTSD screening programme urgently needed”, UCL, Covid Trauma Response Group (2020). Available online at: https://www.ucl.ac.uk/news/2020/jun/covid-19-national-ptsd-screening-programme-urgently-needed
Wallbank S (2012). “Health visitors’ needs – a national perspective from the restorative clinical supervision programme”, Community Practitioner, 85 4, pp.26-29. Available online at: https://www.researchgate.net/publication/224964314_Health_visitors’_needs–national_perspectives_from_the_Restorative_Clinical_Supervision_Programme
Warner C, Appenzeller G, Parker J, Warner C, Hoge C (2011). “Effectiveness of mental health screening and coordination of in-theatre care prior to deployment to Iraq: a cohort study”. American Journal of Psychiatry. 2011; 168: pp.378–85. Available online at: https://pubmed.ncbi.nlm.nih.gov/21245086/
Sign up to our weekly round-up of HR news and guidance
Receive the Personnel Today Direct e-newsletter every Wednesday
WHO (1994) “Declaration on Occupational Health for All”, Geneva, World Health Organization. Available online at: https://www.who.int/occupational_health/en/oehdeclaration94e.pdf?ua=1
WHO (?2008)?. “PRIMA-EF: guidance on the European framework for psychosocial risk management: a resource for employer and worker representatives”. World Health Organization. Available online at: https://www.who.int/occupational_health/publications/PRIMA-EF%20Guidance_9.pdf
