March’s Royal College of Nursing/Society of Occupational Medicine occupational health conference, this year in a virtual format, provided a valuable update on the Nursing and Midwifery Council’s review of the Specialist Community Public Health Nursing (SCPHN) standards, with a public consultation also now set to feed in to the regulator’s future vision for OH. Nic Paton listened in.
It says something for just how much the world has changed after a year of pandemic and lockdowns, but also how much we’re all desperately missing ‘normality’, that the early days of the Nursing and Midwifery Council’s re-evaluation of the Specialist Community Public Health Nursing (SCPHN) standards now have something of an other-worldly quality about them.
As Anne Trotter, the regulator’s assistant director for education and standards, laughingly put it: “We actually managed to have one meeting before the very first lockdown where we met each other, in a room, ate crusty sandwiches and drank coffee!”
NMC SCPHN review
New-look training could be on the cards for OH, as NMC outlines review of SCPHN standards
OH nurses around the table to review Part 3 of the NMC register
Trotter was speaking at March’s Royal College of Nursing/Society of Occupational Medicine occupational health conference, which had been rescheduled from its usual late autumn slot and, of course, this year had been forced to become a virtual event.
The half-day conference nevertheless managed to pack in a lot, with presentations examining the mental health of nurses, the fundamentals of occupational health nursing, leadership within the profession, and a panel discussion on issues facing occupational health as we move through, and hopefully out, of the pandemic.
Declining numbers of SCPHN nurses on the register
Alongside all this, the morning session led by Trotter, who has been leading the NMC’s review of SCPHN standards, and accompanied by Deborah Edmunds, the independent chair representing OH as part of the review and, in her “day job”, global vice president for health risk management and workplace adjustments at Barclays, provided a valuable update on the NMC’s SCPHN review as well as an insight into its potential future thinking on this issue.
To recap, however, the NMC has since 2016 been reviewing both pre-registration and post-registration nursing education and standards. Part of this, at least within OH, has been prompted by long-standing concerns as to whether NMC-validated SCPHN OH courses remain fit for purpose and whether how the NMC can future-proof these to reflect contemporary OH practice.
A first meeting of the steering group looking at the future shape of Part 3 of the register, the current home in terms of registration for many occupational health nurses, was held in December 2019, including with OH representation. It was followed by a second meeting in January 2020 – the final physical meeting Trotter was referring to – again with OH at the table.
While, naturally, much of the work since then has had to be done virtually, Trotter explained to conference delegates that it had been a genuine learning curve. “It has been an incredible and rewarding journey for me; it has opened my eyes up to so much of the knowledge and skills that occupational health nurses are carrying out every day in their day-to-day practice,” she said.
She highlighted one of the key drivers for the need for reform, the fact the number of SCPHN nurses on the register, and alongside that OH nurses, has been falling steadily for some time, albeit only slowly (as shown below). In March 2016, for example, there were 31,158 SCPHN nurses on the register, including 3,516 OH nurses. By March last year, these numbers were 30,392 and 3,220 respectively.
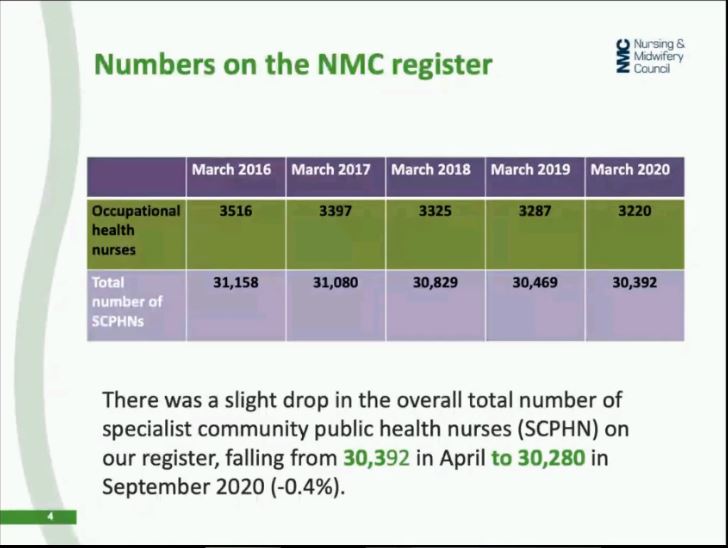
“Although the numbers don’t dwindle by much each year, it is a downward trend over the last five years. We do know that other nurses are working as occupational health nurses without the SCPHN qualification. So, it is an opportunity for us to think about what is important and what SCPHN brings to practice; and what employers can see and benefit from for those with this qualification,” Trotter pointed out.
The review is also looking at community nursing, health visiting and school nursing, with three independent chairs appointed to lead on each. It is examining what can still work or needs to be changed across the piece but also what is distinct about the different disciplines and needs to be considered discretely.
Role of OH now, but also in the future
The NMC has also recognised the review needs to be future-facing. “This is not about what people do now, even though that it is important. It is about what might they need to know? What might they need to be able to do in the future? What would influencing practice look like in one, three, five years’ time?” said Trotter.
It is really important that, when we are thinking about our practice, we actually underpinning it and we know there is fundamental evidence behind what we are doing. It is absolutely imperative that we are champions for health and wellbeing, and that we are actually looking to seek to improve health and improve health outcomes.” – Deborah Edmunds
Within this, the review is examining education and training but also issues such as the role, and future, of prescribing within both SCPHN and OH nursing. The review has been wide-ranging, encompassing an independent verification of the current standards, published in 2019, a review of the situation across the different countries of the UK, a review of academic literature, including internationally, and examination of what sort of regulation is needed in the future.
The impact of the pandemic on health and wellbeing and health inequalities has, naturally, also now had to come into the frame for discussion. There has been a raft of pre-consultation events, with more than 40 held in 2020 alone. The review has even broken the NMC record for its biggest webinar ever held, with some 700 attendees.
So, clearly, there is no shortage of interest. Moreover, as Deborah Edmunds emphasised, a key part of the process has been ensuring the voice of OH has been heard and understood, and that the differences of OH to others within SCPHN has been clearly articulated.
Edmunds during the course of the presentation also outlined the NMC’s future vision for SCPHN and, alongside that, its future vision for occupational health nursing within SCPHN.
SCPHN nurses and midwives, she emphasised, should be autonomous practitioners, be able to practice independently and be driven by evidence and research. ‘We must be capable of adapting a life course approach to professional practice, one that is considerate and inclusive,’ she highlighted.
“It is really important that, when we are thinking about our practice, we actually underpin it and we know there is fundamental evidence behind what we are doing. It is absolutely imperative that we are champions for health and wellbeing, and that we are actually looking to seek to improve health and improve health outcomes. And know how to, and can, effect change that reduces health inequalities. We must be able to, and be, excellent communicators and educators. And be complete leaders and collaborators in creating and implementing strategies for policies to ensure these interventions have a positive effect on people, families and the communities that we serve. And we have to be advisers in safety and quality practice in delivery,” she said.
Vision for OH within SCPHN
The vision for OH within SCPHN (as shown below) was very much that OH nurses needed to nurse leaders, people who lead services and are change agents in the working environment now and into the future.
“We have to possess commercial acumen and the skills for strategic planning and influencing,” Edmunds said. “Too often, I hear that occupational health is ‘somewhere over there’, in a corner and actually where it needs to be is in the boardroom or influencing those senior leaders to understand what actually is important in business?
“Productivity and performance are fundamental if we are to have a successful PLC. So, actually, how are we going to translate what we need to be able to do in that working environment? And you can do that if you know how to create business cases, if you know how to develop ROI, and that you can prove that what you are doing makes business sense.
“We must lead on the prevention strategy. What are we doing to minimise risk and take humans away from the hazard? How are we looking at health by design? How are we designing good health in the working environment?” she added.
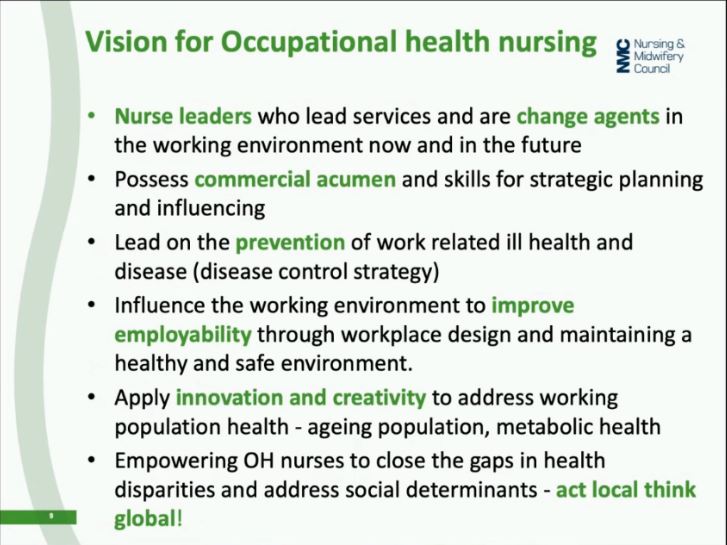
OH also needed to take a lead in terms of thinking about health and wellbeing in the context of employability, especially the multigenerational workplace. Equally, OH had an important role in thinking, and even reimagining, the ageing workforce. As Edmunds put it: “How do we create working environments that enable those with different cognitive functions to be able to flourish? And how do we ensure we are looking at things that really have an impact in terms of population health and around metabolic health?”
Leadership and influencing skills would, increasingly, need to become a core part of the OH nurse’s day-to-day operational toolkit, she argued. “How do you create that narrative; how do you bring it alive? How do you then demonstrate your power, your ability, your capability to actually be that change agent?” she said.
Prescribing needed to be about not just drug or medical prescribing but about social and green prescription and the prescription of work (or ‘good’ work) as a potentially positive health outcome in its own right. “Does our profession have a requirement to, in parts, prescribe? For example if you are working offshore? Or if you are working in an environment where you might be exposing somebody to something, and they need prophylaxis afterwards, why do we allow that to be picked up afterwards by the NHS?” Edmunds said.
“Is there a role for the occupational health nurse to prescribe? For some that might be no, but is that something that other occupational health nurses have a requirement to do and, if so, let’s understand what that might mean?” she added.
All of which brought us to the nub of the event – what happens now? The fact that the review had, up to now, proved so popular in terms of engagement was hugely positive. But the review was now at a point where OH nurses and, indeed, the general public needed to have their say, outlined Trotter.
Launch of widescale consultation
To that end, the next important stage of the review was the launch last month of mass public consultation. The good news too is that, as you’re reading this, it is still open, as the review is running for an extended 16-week period rather than the NMC’s normal 12-week process. That means it closes for responses at the beginning of August, meaning there is still ample time for practitioners to make sure their voice is heard.
The consultation contains an overview document and draft standards and the process will include a survey of people from professional backgrounds, including nurses, OH practitioners, midwives, physiotherapists, dieticians, doctors, and social worker, among others.
There is a consultation survey for members of the general public running alongside, to gauge opinions and views about what they think OH nurses need to know and be able to do. There is also an easy-read version for people with learning disabilities, and a version that has been translated into Welsh. Finally, there will be a series of qualitative in-depth interviews and focus group discussions carried out with members of the public and seldom-heard groups plus a number of NMC engagement events happening during the consultation period.
Sign up to our weekly round-up of HR news and guidance
Receive the Personnel Today Direct e-newsletter every Wednesday
As Trotter put it in conclusion: “So really, this is a plea from me: get involved. We need your voice; Deborah and I cannot do this without you. We need you to tell us what we’ve missed, what’s great, what would make them better. And to do that we need you to participate.”
How to get involved
The consultation can be found at https://www.nmc.org.uk/about-us/consultations/current-consultations/future-community-nurse/
