Four out of 10 doctors feel unable to cope with their workload each week and a quarter are at “high risk” of burnout, the General Medical Council (GMC) has warned.
The GMC study, The state of medical education and practice in the UK: workplace experiences 2023, was published just ahead it being revealed that senior doctors will go on an unprecedented 48-hour strike later this month.
The GMC has tracked doctors’ workplace experiences since 2019, and the latest survey showed a continuing deterioration since the pandemic hit in 2020, with doctors’ experiences “now worse than at any time since we began the Barometer survey”, it said.
Just 50% said they were satisfied in 2022, down from 70% in 2021. In 2022, more doctors reported working beyond their rostered hours on a weekly basis (70%, up from 59% in 2021), having difficulty taking breaks each week (68%, up from 49% in 2021), and feeling unable to cope with their workload each week (42%, up from 30% in 2021)..
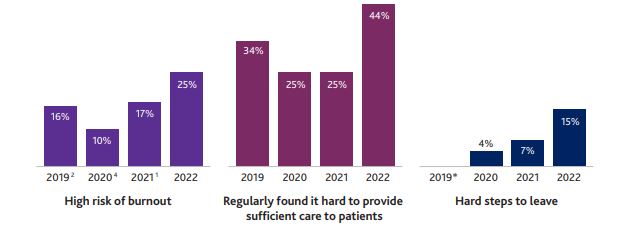
A quarter of doctors surveyed (25%) were categorised as being at high risk of burnout in 2022, compared with 17% in 2021, the GMC warned (see graphic below).
The GMC finding is also broadly in line with last month’s 2022 annual consultant physician workforce census, carried out by the Royal College of Physicians of London, Royal College of Physicians of Edinburgh and Royal College of Physicians and Surgeons of Glasgow.
This found almost one in five doctors (18%) almost never feel in control of their workload and were at risk of burnout, while 44% reported having an excessive workload almost always or most of the time.
Medical profession burnout
This was having a knock-on effect on the quality of patient care, the GMC study warned. In 2022, more than two-fifths of doctors (44%) said they found it difficult to provide sufficient patient care at least once a week. This was a significant increase from 2021, when a quarter of doctors (25%) reported this, and 2019, when a third of doctors said the same (34%).
The situation was contributing towards a mass exodus of staff from the NHS, so creating a vicious cycle.
More doctors than ever said they were likely to leave the UK profession and had taken hard steps towards doing so (excluding doctors of retirement age who were planning to retire), the GMC said. A total of 15% of doctors said they had taken steps to leave, up from 7% in 2021.
GPs also reported poor, and worsening, workplace experiences. In 2022, 38% of GPs said they were satisfied, fewer than other doctors and down from 51% in 2021.
More half of GPs (55%) were categorised as struggling with their workload, compared with 38% of all doctors.
Equally, fewer disabled doctors were satisfied with their work, 44% compared with 51% of non-disabled doctors. Almost half (47%) of disabled doctors were categorised as struggling with their workload, compared with 37% of non-disabled doctors, the GMC added.
Charlie Massey, GMC chief executive, warned the findings showed the NHS workforce plan, which intends to expand the NHS workforce, needed to be backed with more work on supporting the health and wellbeing of those who will need to train and support these new entrants.
‘More clinicians than ever are telling us they are taking steps to leave the profession, and the gap they could leave behind will only compound workload pressures and feed into a vicious cycle,” he said.
“It’s especially worrying to see the impact on trainers, who are critical for ensuring that our doctors in training develop the skills and confidence they need. Any government commitments to expand medical training places, whilst welcome, will flounder if the needs of the trainer workforce are not urgently met.”
In response, the Nursing and Midwifery Council (NMC) pointed out that there is a similar, and worsening, picture in nursing, too.
It reported in May that more than half of those who left the nursing and midwifery register last year did so earlier than planned.
Sign up to our weekly round-up of HR news and guidance
Receive the Personnel Today Direct e-newsletter every Wednesday
There were five compounding workplace factors influencing this, it argued: burnout or exhaustion; lack of support from colleagues; concerns about the quality of people’s care; workload; and staffing levels.
Andrea Sutcliffe, NMC chief executive and registrar, said: “The fact that burnout and high workloads are driving away doctors echoes the factors that cause many of our own professionals to leave, taking vital knowledge and skills that improve people’s health and wellbeing with them. And the fact that doctors from ethnic minorities feel less supported is further evidence of the need for employers everywhere to foster inclusive, anti-racist cultures that support all professionals to thrive.”